Beyond Grey’s Anatomy: What Medical Training Actually Looks Like
⌚️ read time: 6.2 minutes
At dinner parties, when the topic of careers comes up, I am often asked what the path is to becoming a hand surgeon. Or a doctor in general.
Given how frequently I’m asked, it’s likely a few of you have wondered the same. If you’re at all curious about the current process of medical training, this one’s for you.
So here goes!
The College Years (4 years)
Like many, I certainly look back fondly on my college years, but there’s no doubt these memories also come with a tinge of dread.
Never will I miss the brutality of courses like organic chemistry and physics — courses nicknamed "weed-out classes" because of their notorious difficulty and propensity for squashing dreams of medical careers before they ever begin.
I consider these class requirements to be the first ‘artificial’ hurdle in a long line of ‘prove yourself’ requirements on the path to becoming an MD.
Bleh.
As doctor shortages begin to rear their ugly heads around the country…why on earth are we discouraging so many from pursuing this field? And I fear that with so many changes making healthcare careers less desirable, the shortages will only worsen…
But I digress.
In these early years, undergraduates don’t actually need to choose a "pre-med" or science major. Any major works, as long as you complete the prerequisite courses and maintain strong grades.
In fact, I now very much wish I had majored in something other than science. When else in your life do you get the opportunity to throw yourself into mastering a subject? The science was always going to be there as the medical school prerequisite.
And, of course, near the end of college, most of my free time was spent studying for the MCAT (Medical College Admission Test). This 7.5-hour exam covers everything from chemistry to critical thinking, and it's another big early hurdle that will be an important part of your medical school application.
Medical School (4-5 years)
Unfortunately, even as we experience the above-mentioned doctor shortages, medical schools are becoming increasingly difficult to get into. The admission rates are appalling.
Once you do get in, most medical schools start with two years of intensive classroom learning.
Ever tried learning a new language?
Medical students reportedly learn about 30,000 new terms during these first two years. You're memorizing every nerve, muscle, and bone in the body, not yet knowing which ones will become most relevant to your future specialty.
The third and fourth years then switch to hospital rotations. One month you're in the pediatric ward, the next you're assisting in the operating room. These rotations help you figure out which field of medicine calls to you.
For some, it's the precise work of surgery; for others, it's the long-term relationships built in primary care.
Between these clinical rotations, you're studying for two major licensing exams (USMLE Step 1 and Step 2). These scores play a huge role in determining which residency programs might accept you.
When I went through, Step 1 was an epic make-or-break test that essentially determined which specialties you were competitive enough to apply for. My school literally gave us 6 weeks off JUST to study for this exam.
The pressure was enormous.
It’s my understanding that this has changed somewhat to smooth out the importance of multiple exams over time, rather than having it all come down to one. I’m sure there are pros and cons to this new approach.
The Match System
At the end of medical school, the goal is to continue the next phase of medical training in what is called ‘residency.’
But rather than a standard application/acceptance process, residency placement works through a process called "The Match." This is an algorithm that pairs graduating medical students with residency programs.
To prepare, you spend much of the 4th year of medical school doing ‘visiting internship’ months at hospitals you think you might like, surfing couches, and generally living out of a suitcase. Once those are done, the rest of the year is spent completing formal residency interviews across the country.
Come spring, you rank your preferred programs, and each hospital ranks their preferred candidates. A computer algorithm then ‘matches’ everybody’s preferences accordingly.
To be clear, this process was invented to ensure hospitals get the residents (cough, cheap, subsidized labor) they need rather than having multiple empty slots at the end of the process. Empty slots would mean the hospital would have to go hire an expensive nurse practitioner, physician’s assistant, or doctor to perform the duties a typical resident would typically complete.
Here’s another kicker. This Match process is 100% legally binding — whether you like the location you are given or not.
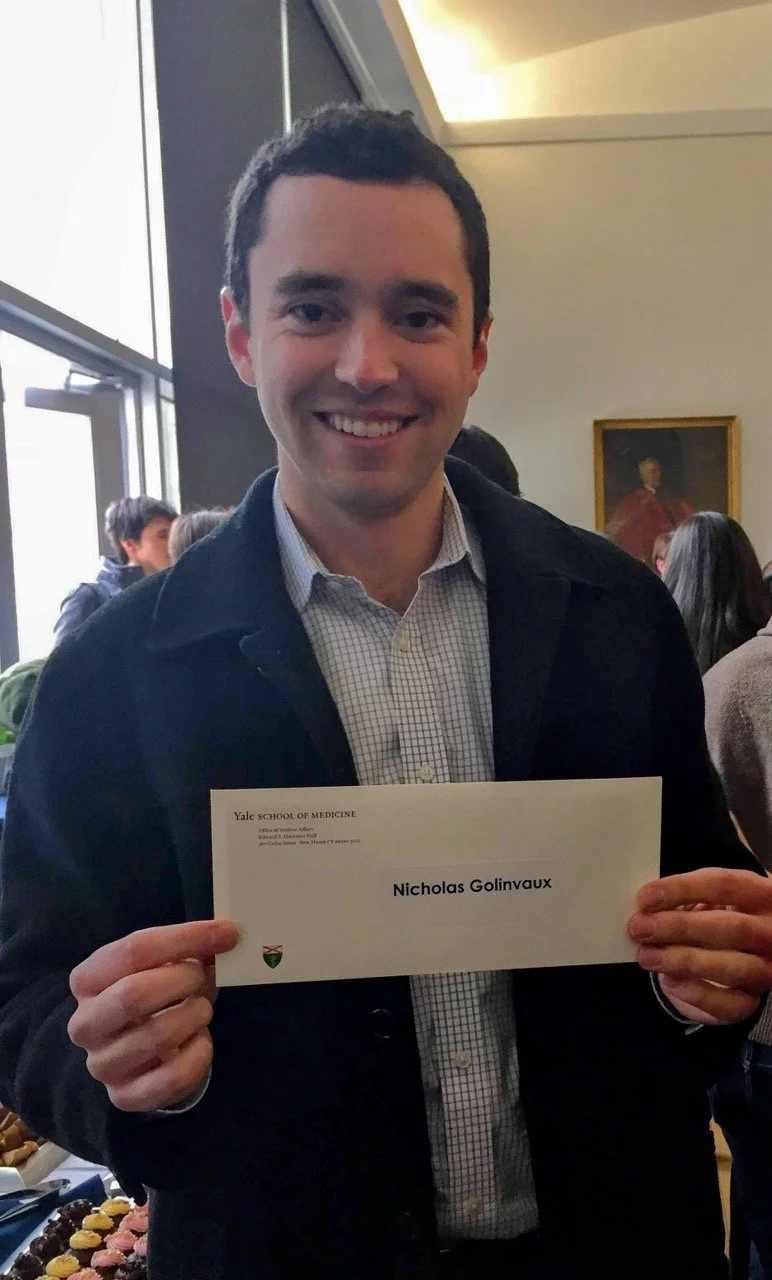
For obvious reasons, this process has become somewhat legendary. Mostly because there comes a single moment in time (I remember mine vividly) when you pick up your Match envelope, knowing full well that once you open it, you will be told where to pick up and move to spend the next 5 years of your life.
For some, it’s elation (I’m thankful every day this was how it played out for me). For others, it can be devastating (😔).
High drama.
Look at that fake smile full of nerves
Orthopedic Surgery Residency (5 years)
Ah residency. It was the best of times, it was the worst of times.
During residency, you’re officially a doctor. But this is where the real training and learning begins.
(For those following along, residency is where the famous TV show Grey’s Anatomy begins).
Surgical residency starts with intern year — sort of a crash course in basic surgical principles and patient care.
In fact, even though I was an orthopedic surgery resident, I basically belonged to the general surgery department during intern year. I worked on services like vascular surgery, general surgery, and oncology. This is when you truly learn how to care for hospitalized patients.
Once you pass intern year, the following four years focus solely on orthopedic surgery, gradually increasing in complexity and responsibility.
In the early years, you slog it out in the emergency room, seeing and treating orthopedic injury after orthopedic injury. Think shattered pelvises in car accidents, missing arms after golf cart rollovers, and paralyzing gunshot wounds to the spine. These were sprinkled amongst a steady stream of run-of-the-mill injuries like kids falling off monkey bars, avocado hand injuries, and infections.
These years are a blur. Depending on where you train, the sheer volume can be wild. I chose an extremely busy training program — and my personal record to show for it was 39 separate orthopedic consults in a 24-hour period.
And in one instance, I saw 25 in a single 12-hour night. That night, I sat down to record the patient details of a page that came across my beeper. And it just kept beeping. I actually thought it was broken. Before I finished writing, I had not one…not two…not three…but six fresh consults to race off and treat.
Talk about cold sweat dripping down your neck.
Later in residency, you’re no longer patrolling the ER, but spending more time in the operating room. You start by watching simple procedures and work your way up to taking the lead in more difficult surgeries, all under the watchful eye of the ‘attending’ surgeon.
In contrast to everything we know about human health, there’s no doubt that sleep was relegated to an occasional luxury. Most days began before sunrise and ended well after sunset. 28-hour shifts were the norm every few days. The old guard will say this teaches you to operate while tired, think clearly under pressure, and make difficult decisions.
And there’s no doubt that I learned more than I could ever have imagined during residency.
But is there a better balance out there given what we now know about how critical sleep is for healthy brain function?
I don’t know the answer. Maybe residency needs to be 10 years instead of just 5 (😱).
All I know is that if you told me today I would have to repeat my residency…I’m not sure I’d have the energy.
Hand Surgery Fellowship (1 year)
Fellowship is like finishing school. During residency, you choose which sub-specialty you’d like to pursue and another ‘Match’ process ensures. For me, I chose a fellowship in hand and upper extremity surgery. We learned to operate on anything from the shoulder down to the fingertips.
This year is spent mastering intricate techniques like microsurgery — connecting tiny blood vessels and nerves under the microscope — and tendon repairs. Because this fellowship spans the entire upper extremity, you learn to treat everything from arthritis to traumatic injuries.
It’s still a lot of work, but for me it was by far the most enjoyable aspect of training given the choice I made to be there.
Board Certification (∞)
Once you’ve graduated fellowship, you’re officially an independent surgeon, and you go on your merry way, right?
Wrong.
Throughout this journey from medical school onwards, you face a series of board examinations. These ensure you've mastered the knowledge and skills needed for independent practice.
After all, this makes sense for those who make it a career to cut open patients’ arms and legs.
This board certification process begins with the Step 1 and 2 exams I mentioned during medical school. During the intern year of residency, you complete Step 3 and you officially become licensed with the USMLE (some long acronym).
But then come orthopedic surgery boards. The big ones.
This involves another long written test following residency. If you pass that, you then wait until completing 2 years of independent practice following fellowship before submitting 6 full months of all the surgical cases you do to the Board.
The journey never ends!
If you do well on those 6 months of case review, you then fly to Chicago and, quite honestly, get grilled for 4 hours about 12 specific cases they choose. Passing this exam gets you officially board-certified as an orthopedic surgeon. Woohoo!
But wait, there’s more!
To become a certified hand surgeon, there are another 6 months of cases to submit, followed by a final written test, usually taken after about 5 years in practice.
After all this? You’re. Finally. Done.
Well, except when you need to re-certify every ten years...😂.
A few brief thoughts
Looking back, every year of training added crucial skills and knowledge. Modern hand surgery combines elements of orthopedics, plastic surgery, and microsurgery. It requires both technical precision and decision-making ability. While the path is long, it provides the foundation needed to help patients regain function and return to their daily activities.
For anyone considering this path: Yes, becoming a doctor is a significant commitment. Of time, energy…and finances. Each step, test, and flight outlined above is something the trainee pays for. We should explore this more in another article, but what does this do to the potential field of applicants?
Honestly, I wish I had understood it a bit better on the front end to know what I was getting into.
But. If you're fascinated by the intricate workings of the human body and driven to help others? It's a hard field to beat.
Takeaways:
There’s no denying that medical training is a long slog, gradually progressing from broad knowledge to specialized expertise
This progression combines demanding hours, mountains of information, and a heavy burden of examinations that must be passed to move on to the next step
Even once a doctor reaches independent practice, board certification requires ongoing re-certification, ensuring maintenance of competency and learning throughout one’s career
At the end of the day, it’s hard to beat a career founded on helping others and a lifelong pursuit of understanding the human body